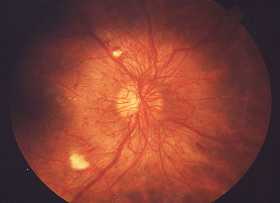
Diabetic retinopathy,is retinopathy (damage to the retina) caused by complications of diabetes, which can eventually lead to blindness.
Classification
Non-proliferative : Retinopathy, Maculopathy
Proliferative Retinopathy
Non-Proliferative Retinopathy
Manifestations:
Mild : At least one microaneurysm
Moderate :
- Extensive microaneurysm
- Intraretinal haemorrhages
- Venous beading
- Cotton wool spots
Severe :
- Cotton wool spots
- Venous beading
- Intraretinal Microavascular Abnormalities (IRMA)
Nonproliferative Maculopathy
Manifested by focal or diffuse retinal thickening or edema due to breakdown of the inner blood retinal capillary endothelium causes leakage of fluid and plasma into surrounding of retina.
More common in type II diabetes which requires treatment once significant which is confirmed by any retinal thickening within 500 microns of the fovea, hard exudates withing 500 micron of the fovea with retinal thickening. Also retinal thickening greater than one disc diameter in size
It may due to schema which is characterized by macular edema, deep haemorrhages and little exudation.
Fluorescein angiography shows loss of retinal capillaries with enlargement of the foveal avascular zone.
Proliferative Retinopathy
It is the most severe complications of Diabetes
It is characterised by NVD & NVE
Diagnosis
Diabetic retinopathy is detected during an eye examination that includes:
- Visual acuity test: This test uses an eye chart to measure how well a person sees at various distances (i.e., visual acuity).
- Pupil dilation: The eye care professional places drops into the eye to widen the pupil. This allows him or her to see more of the retina and look for signs of diabetic retinopathy. After the examination, close-up vision may remain blurred for several hours.
- Ophthalmoscopy or fundus photography: Ophthalmoscopy is an examination of the retina in which the eye care professional:
- looks through a slit lamp biomicroscope with a special magnifying lens that provides a narrow view of the retina.
- wearing a headset (indirect ophthalmoscope) with a bright light, looks through a special magnifying glass and gains a wide view of the retina. Hand-held ophthalmoscopy is insufficient to rule out significant and treatable diabetic retinopathy. Fundus photography generally recreate considerably larger areas of the fundus, and has the advantage of photo documentation for future reference, as well as availing the image to be examined by a specialist at another location and/or time.
- Fundus Fluorescein angiography (FFA): This is an imaging technique which relies on the circulation of Fluorescein dye in the eye vasculature.
- Optical coherence tomography (OCT): This is an optical imaging modality based upon interference, and analogous to ultrasound. It produces cross-sectional images of the retina (B-scans) which can be used to measure the thickness of the retina and to resolve its major layers, allowing the observation of swelling and or leakage.
- Digital Retinal Screening Programs: Systematic programs for the early detection of eye disease including diabetic retinopathy are becoming more common, such as in the UK, where all people with diabetes mellitus are offered retinal screening at least annually. This involves digital image capture and transmission of the images to a digital reading center for evaluation and treatment referral.
- Slit Lamp Biomicroscopy Retinal Screening Programs: Systematic programs for the early detection of diabetic retinopathy using slit-lamp biomicroscopy. These exist either as a standalone scheme or as part of the Digital program where the digital photograph was considered to lack enough clarity for detection and/or diagnosis of any retinal abnormality.
The eye care professional will look at the retina for early signs of the disease, such as:
- leaking blood vessels
- retinal swelling, such as macular edema
- pale, fatty deposits on the retina (exudates) – signs of leaking blood vessels
- damaged nerve tissue (neuropathy)
- any changes in the blood vessels.
Should the doctor suspect macular edema, he or she may perform fluorescein angiography and sometimes OCT.
Treatment and Management
- Laser photocoagulation
- Modified Grid Laser photocoagulation
- Panretinal photocoagulation
- Intravitreal triamcinolone acetonide
- Intravitreal Anti-VEGF
- Vitrectomy
References:
- Vaughan & Asbury's General Opthalmolgy 17th Edition
- http://en.wikipedia.org/wiki/Diabetic_retinopathy